Clinical history : 36/ F history of left sided gradual onset proptosis with diplopia
IMAGING FINDINGS:
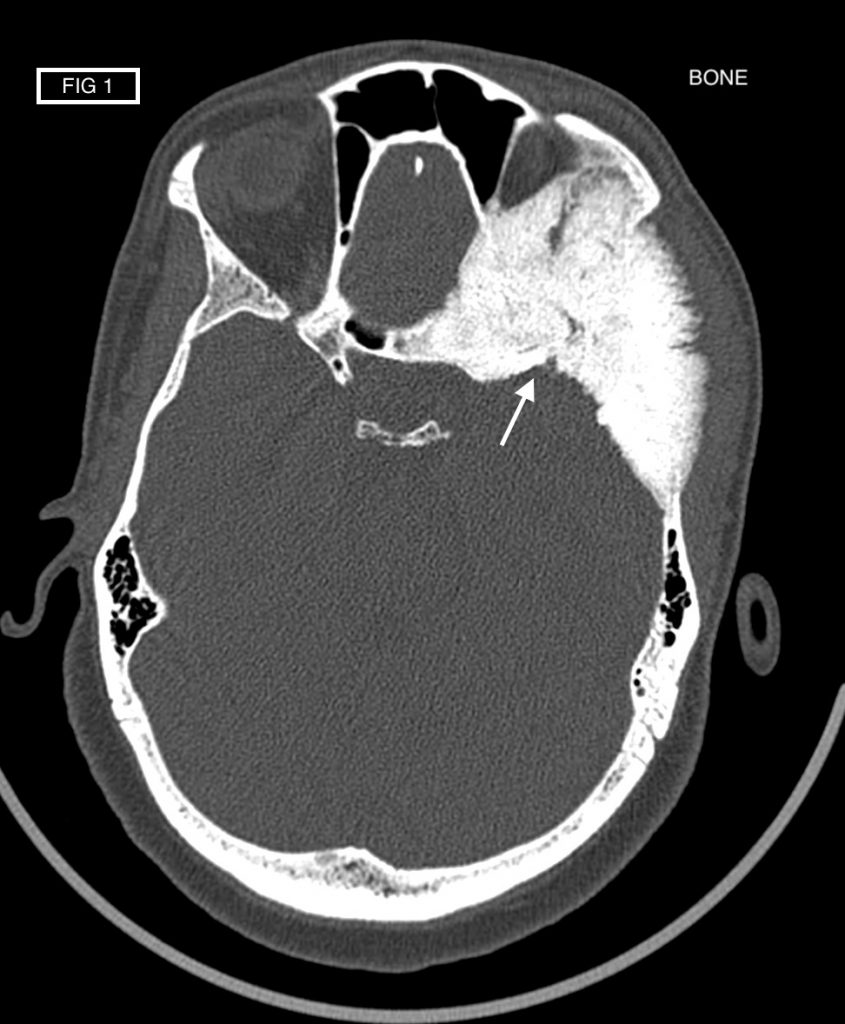
- Marked hyperostosis seen in the left frontal and temporal bones, extending into sphenoid wing, superior / lateral walls of left orbit and lateral wall of posterior ethmoid and sphenoid sinus, on left side. Displacement of lateral rectus muscle & moderate degree of proptosis noted.
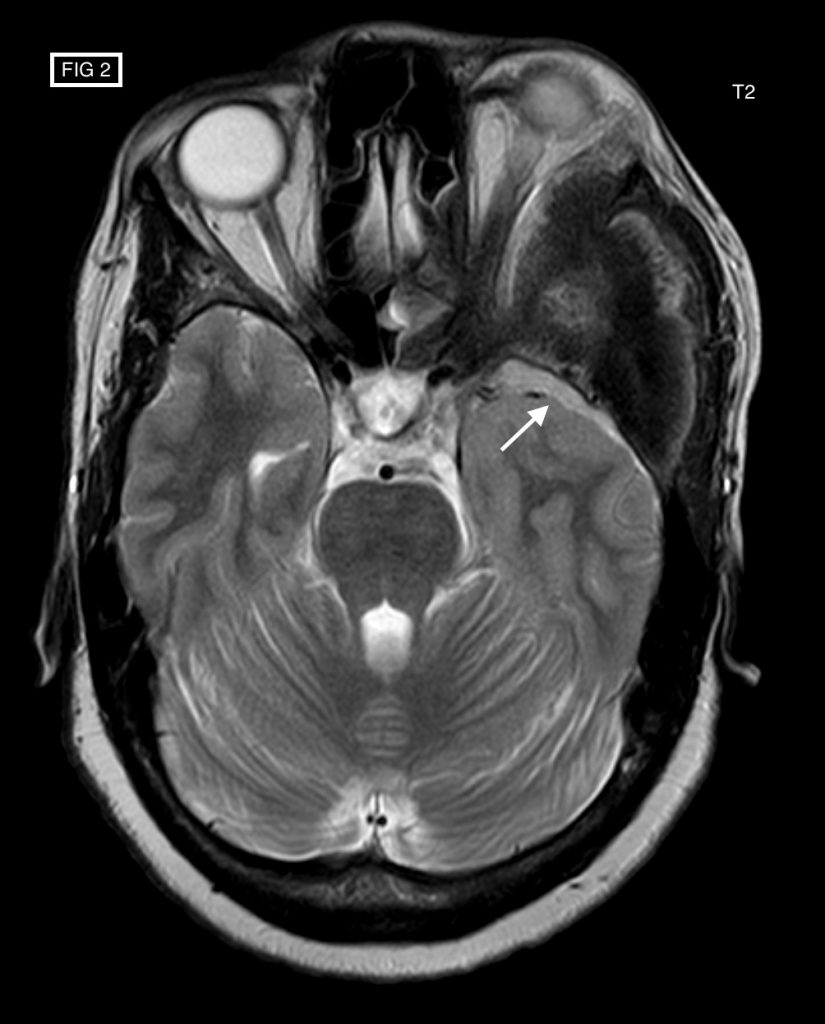
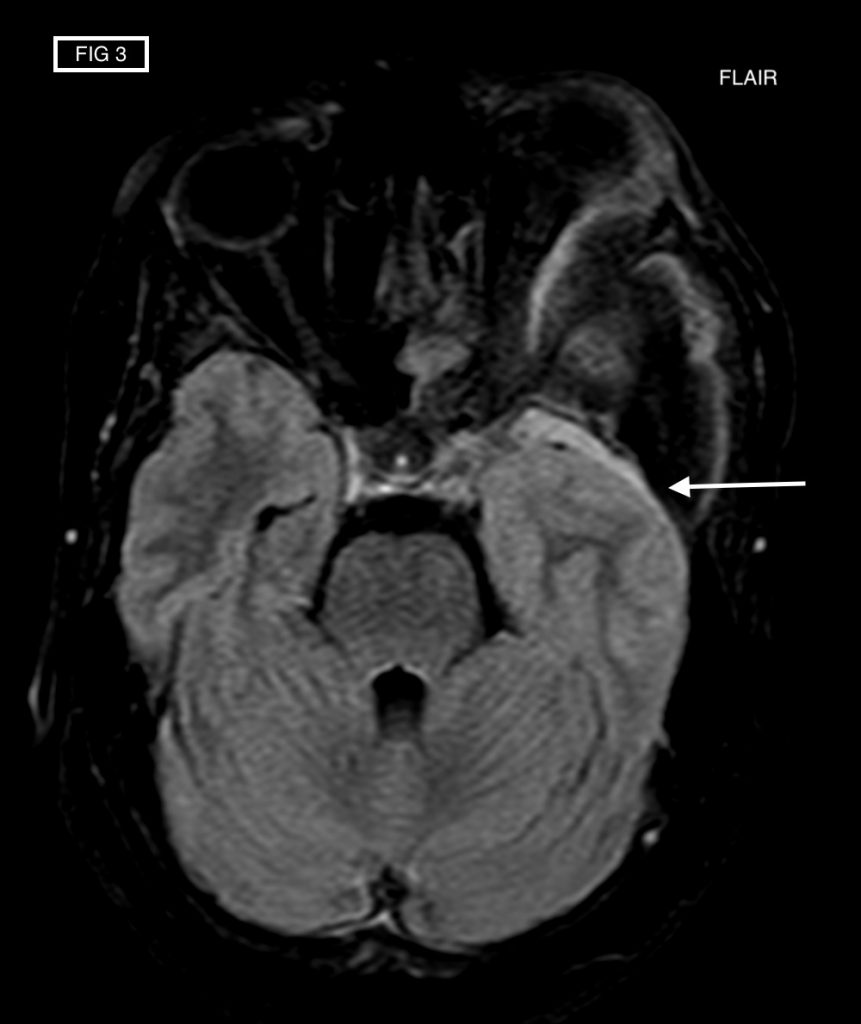
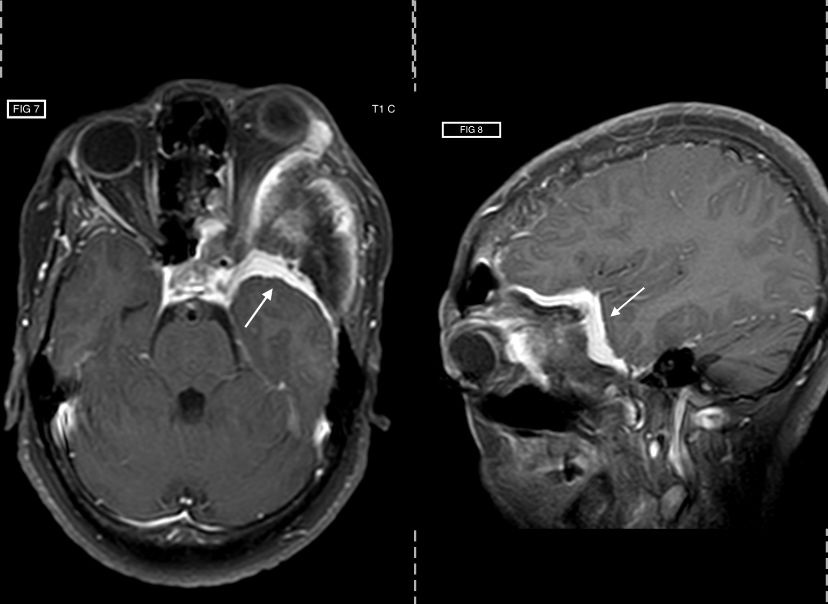
- Flat dural thickening, appearing iso-intense on T1-weighted images & iso-to-hyperintense on T2-weighted images, noted in left frontal-temporal convexity adjacent to the bone changes. Transgression across the sclerotic bone noted with extra-calvarial involvement.
- Indentation and compression of adjacent brain parenchyma seen. However, no demonstrable oedema seen on T2/ FLAIR images.
- The lesion shows intense & homogeneous post contrast enhancement.
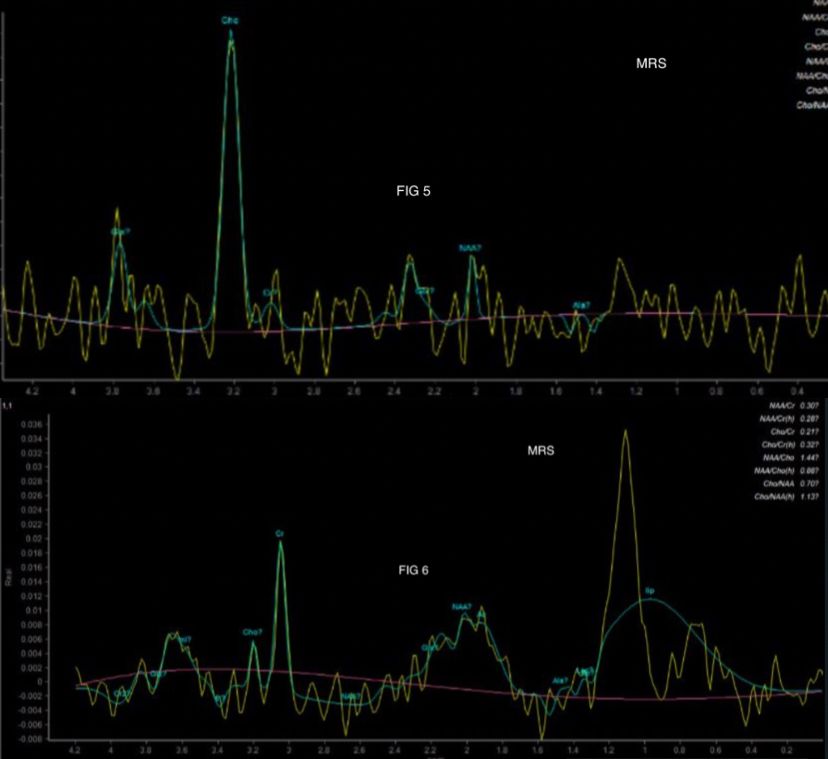
- Elevated lipid peak (in short TE) + alanine doublet inversion at 1.4 ppm (long TE) + Distinct peak at 3.8 ppm (long TE) – Noted in MRS.
IMAGING FEATURES ARE CONSISTENT WITH MENINGIOMA EN PLAQUE
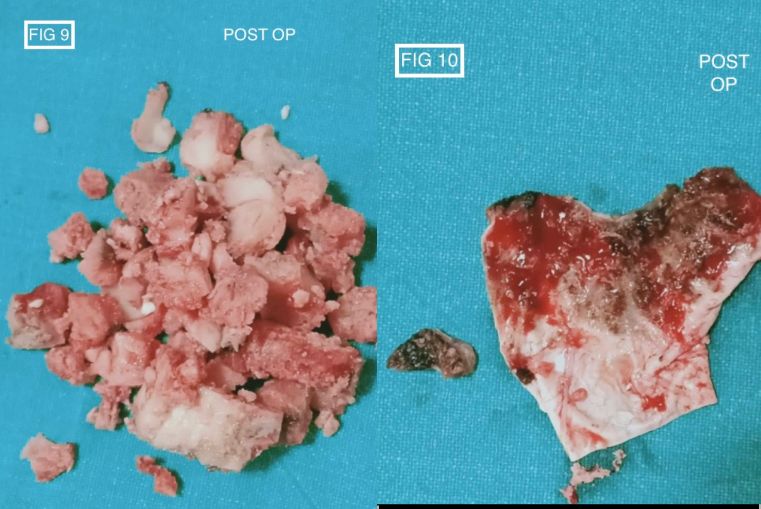
- Complete tumour excision is necessary to prevent recurrence. But most times, complete resection is impossible due to the close proximity of vital structures. The intra-operative images are attached showing the dura with tumour and the excised bony components of the lesion.
DISCUSSION :
The term ‘meningioma en plaque (MEP)’ was coined by Cushing and Eisenhardt in 1938 to differentiate these uncommon sheet-like meningiomas from the more common globular variety, ‘meningioma en masse’.
They constitute 2-4 % of all intracranial meningiomas. Morphologically these are carpet or sheet-like lesions that grow in a radial fashion along the meninges. They tend to invade the adjacent bone resulting in bony hyperostosis which is disproportionately greater than the size of the intracranial mass itself. Hence, Unlike in globular meningiomas, the bony hyperostosis in meningiomas en plaque is more likely to be secondary to tumour invasion. Although locally invasive, they usually correspond to a WHO grade I meningioma.
Contrast enhanced MRI is the preferred imaging modality. En plaque meningiomas may have a varied appearances, ranging from a smooth thin extra-axial mass to a highly irregular lobulated lesion. The lesion tends to grow radially or in a sheet-like manner along the dura, as described in our case above, with prominent calvarial thickening. CT is always superior to demonstrate the osseous changes.
Hyperostosis of the skull associated with MEP is often confused with other hyperostosing conditions such as fibrous dysplasia (FD) and osteoma.
Unlike FD, which is characterised by ground glass matrix, the hyperostosis in MEP is characterised by indolent growth and a sclerotic pattern. Periosteal hyperostosis pattern when seen in MEP can confidently differentiate this condition from FD, as periosteal new bone formation is not seen in later. Another clue is, the surface of the bony hyperostosis is irregular in MEP whereas it is smooth in FD. In FD, the curvature of the inner table is usually preserved and the pressure effect on the adjacent brain is unusual.
Osteoma usually arises from the outer table of the skull and rarely from the inner table, but as a rule, does not extend into the diploe. A biconvex appearance with inward and outward bulging has not been reported in osteoma and is characteristic of MEP. Another differential point is that osteomas do not extend across suture lines, whereas hyperostosis from MEP may do.
Dural metastasis can appear as focal nodular dural thickening or as diffuse smooth dural thickening showing intense enhancement like meningioma on post contrast study. In such scenario MR spectroscopy could help as metastases have high choline, low NAA:creatine ratios and high lipid:creatine ratios without the alanine peak, which is characteristic of meningiomas, as shown in our case.
Diffuse dural lymphoma cam mimic MEP, as these highly cellular neoplasm appear hyper dense on CT and show intense homogeneous post contrast enhancement. However, they show restricted diffusion more often than meningioma or metastases. MR perfusion will be also be helpful in these cases.
To conclude, en plaque meningiomas are a rare flat variety of intracranial meningiomas which grow along the planes of the meninges. Their diagnosis remains difficult but should be considered when linear or lobulated enhancing dural-based mass lesion is seen with disproportionate underlying bone changes.