A 29-year-old male patient presented with history of fever, headache, abdominal pain and acute onset of altered sensorium. On neurological examination, patient had cognitive impairment and no evidence of neck rigidity.
Cerebellar involvement could not be evaluated clinically, as the patient was in a state of altered sensorium. Lab values showed thrombocytopenia. The diagnosis of dengue was confirmed by positive serology for Ig-M antibody and NS- 1 antigen. There was no history of hypertension. Blood pressure was normal at the time of admission.
Final Diagnosis: Haemorrhagic dengue encephalitis
Imaging Findings:
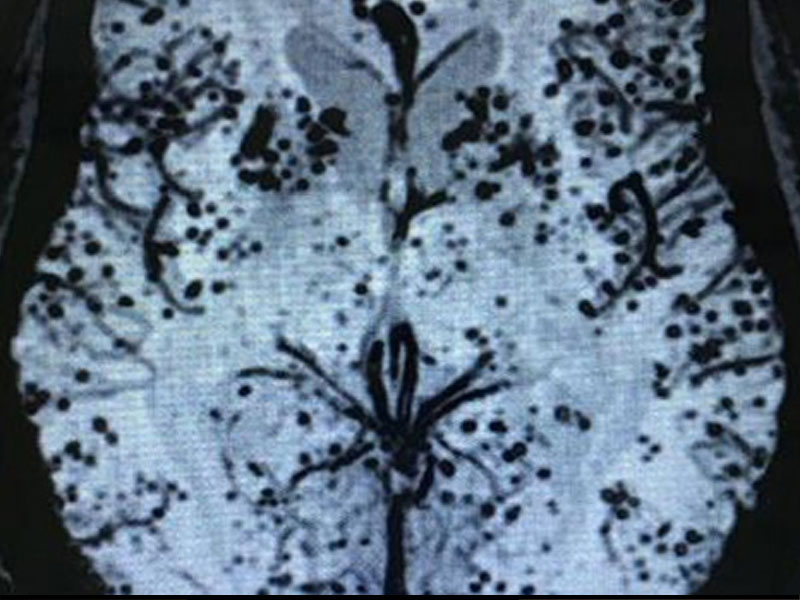
Initial imaging with ultrasound (US) and computed tomography (CT) was done. USG abdomen showed gall bladder wall oedema, ascites and bilateral pleural effusion. Non-contrast CT brain showed hypodensity in bilateral capsuloganglionic regions (Fig. 1). MRI was advised with the suspicion of dengue encephalitis and it showed areas of T2/FLAIR hyperintensities in bilateral capsuloganglionic regions (Fig. 2 and Fig. 3). No significant diffusion restriction was seen. No evidence of haemorrhage seen in T2/FLAIR sequences. However, SWI sequence showed multiple tiny areas of blooming suggestive of microbleeds (Fig. 4). Contrast MRI was not performed in this patient as the consent could not be obtained from the patient attendants. However, CSF analysis did not show signs of menigitis. Follow-up imaging was obtained after three months. Patient had good clinical outcome and corresponding
MRI showed complete resolution of hyperintensities (Fig. 5).
